Dermal exposure
At the Institute of Occupational, Social, and Environmental Medicine at the Friedrich-Alexander-Universität Erlangen-Nürnberg, the working group of Prof. Dr. Göen has developed and validated a measurement strategy for the determination of dermal exposure to hazardous substances; since 2010, this method has been successfully applied in a number of projects.
The quantification of dermal exposure concerns both personal sampling at the level of the worker as well as stationary measurement using a surrogate area. Primarily personal sampling, which comprises potential or actual dermal exposure, provides a valuable contribution to the evaluation of various routes of exposure and thereby helps to comprehensively and correctly describe exposure situations in the workplace.
Further information can be found here
Contact: Dr. rer. nat. Anja Schäferhenrich
„Skin hazards from wearing gloves which are impervious to fluids“
Objective:
Wearing gloves which are impervious to fluids is considered “humid work” (TRGS 401) and, according to ArbMedVV, occupational medical care is required for workers engaging in at least four hours of humid work per day, even if there is no scientific evidence to date to suggest that working with such gloves is significantly damaging to the skin when the workers’ hands are clean and in the absence of hazardous substances (Ochsmann et al. 2006). This study will examine whether workers who regularly work more than 4 hours per day wearing liquid-tight gloves suffer more frequently from skin changes on the hands or whether their skin changes are more severe than workers who do not wear gloves.
Materials and methods:
A collective of workers from the semiconductor industry – workers from the clean room who wear liquid-tight gloves more than 4 hours per day as well as administrative workers to serve as a control group – were included and investigated as part of the study. Alongside glove-wearing behaviour, non-occupational risk factors for hand eczema (gender, smoking, atopy, etc.) were systematically surveyed as part of a standardised interview. The dermatological findings of the hands were measured using the quantitative skin score HEROS; physiological skin parameters for the measurement of subclinical skin damage were investigated via transepidermal water loss (TEWL) and corneometry. Furthermore, polarisation spectroscopy was used as a new investigative instrument for occupational medicine in the field.
Results:
When using the HEROS score, clinical dermatological findings of the hands showed no significant difference when comparing the collectives “glove wearers” vs. “controls”. Transepidermal water loss (TEWL), however, was significantly increased for “glove wearers”. In any case, these changes were no longer detectable about 30 to 40 minutes after glove removal and did not indicate a permanently affected skin barrier. In the multiple linear regression, the duration of activity seemed to be a significant influential factor for the magnitude of TEWL for part of the study collective. “Glove wearers” reported skin diseases on the hands more frequently since beginning work in the clean room. No significant difference in the anamnesis could be found between the collectives regarding relevant skin changes to the hands, such as from hand eczema or signs of atopy, ruling out the possibility of selection bias.
Conclusion:
Our investigations showed that wearing liquid-tight gloves for more than 4 hours per day with clean hands and in the absence of hazardous substances shows no indication of serious effects on the condition of the skin, such that it must be discussed whether clean-room workers require supplementary, symptom-related preventive care in addition to a concrete (clean room-related) skin-protection policy or whether the mandatory preventive care prescribed by ArbMedVV should continue be carried out at fixed intervals.
References:
Weistenhöfer W, Wacker M, Bernet F, Uter W, Drexler H. Occlusive gloves and skin conditions: is there a problem? Results of a cross-sectional study in a semiconductor company. Br J Dermatol 2015; 172 (4): 1058-1065 https://onlinelibrary.wiley.com/doi/full/10.1111/bjd.13481
Weistenhöfer W, Uter W, Drexler H. Has dry/cold weather an impact on the skin condition of cleanroom workers? J Toxicol Environ Health A 2016; 79 (22-23): 1118-1124 https://www.tandfonline.com/doi/full/10.1080/15287394.2016.1219602
Weistenhöfer W, Uter W, Drexler H. Protection during production: Problems due to prevention? Nail and skin condition after prolonged wearing of occlusive gloves. J Toxicol Environ Health A 2017; 80 (7-8): 396-404 https://www.tandfonline.com/doi/full/10.1080/10937404.2017.1304741
Weistenhöfer W, Uter W, Bernet F, Drexler H. The Tissue viability imaging system – suitable method for discovering minimal skin changes in occupational screenings? Results of a cross-sectional field study. Skin Res Technol 2019; 25: 553-563 https://onlinelibrary.wiley.com/doi/full/10.1111/srt.12686
This project was financed by the BG ETEM.
Contact person: PD Dr. med. Wobbeke Weistenhöfer
Our Online UV Anamnesis Tool
https://uv-anamnese.housing.rrze.uni-erlangen.de/Sonnenjahre
Click here for your own personal access code.
Measurement of UV exposure using the Standard Erythema Dosage SED
(1 SED = 100 J/m² (erythema radiation stramght Her))*
-
-
-
- Value A:
age-equivalent UV lifetime dosage for “indoor workers”
(yearly average of 130 SED/year x age at first diagnosis of the skin tumour) - Value C:
generalized supplements and reductions for extreme outdoor/indoor recreational activities - Value B:
additional work-related UV dosage for outdoor workers
► for several work stints, if applicable
► assumption of 170 SED/year as the average additional work-related annual dosage of natural UV radiation and
► consideration of the following factors:
(I) the duration of activity,
(II) the time of activity (summer/winter; midday or morning/evening) and
(III) the location of activity (geographic latitude, sea level, albedo, as well as the
(IV) degree of coverage of the affected skin area
- Value A:
-
-
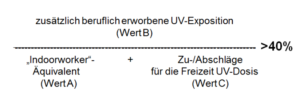 –> possible occupational disease =
–> possible occupational disease =
report of a justifiable suspected case of an occupational disease
Everyone is exposed to solar UV radiation. Based on current scientific knowledge, an additional UV exposure of 40% leads to double the risk (RR = 2) of squamous cell carcinomas. Squamous cell carcinomas and multiple actinic keratosis of the skin may be recognised and compensated as occupational diseases per No. 5103 of the appendix to the German Ordinance on Occupational Diseases, if the location of the tumour required an additional occupational UV exposure of at least 40%. Occupational and non-occupational solar UV exposure must therefore be retrospectively and quantitatively estimated and contextualised in order to determine whether a suspected case of an occupational disease can be reported. The Online UV Anamnesis Tool makes this possible in a reasonable amount of time. Examinations on its application in field studies and validity tests have yielded good results.
Literatur
Weistenhöfer W, Hiller J, Drexler H, Kiesel J. Retrospektive Expositionsabschätzung der natürlichen UV-Strahlendosis: Erfahrungen mit dem Online-UV-Anamnese-Instrument im Feldversuch. J Dtsch Dermatol Ges 2017; 15 (6): 610-620 https://onlinelibrary.wiley.com/doi/full/10.1111/ddg.13250_g
Kiesel J, Wolf V, Knuschke P, Wittlich M, Letzel S, Drexler H. UV-Anamneseauxilium zur Expositionsabschätzung der natürlichen UV-Strahlendosis von im Freien Beschäftigten. Arbmed Sozialmed Umweltmed 2013; 48: 250-253 https://www.asu-arbeitsmedizin.com/wissenschaft/uebersicht-uv-anamneseauxilium-zur-expositionsabschaetzung-der-natuerlichen-uv
This research project was funded by the DGUV (FB 170).
Contact person: PD Dr. med. Wobbeke Weistenhöfer